The traditional denials and appeals (D&A) management process continues to labor under the twin burden of growing costs and complexity. Ongoing reliance on paper records and manual processing not only costs hospitals and patients time and money but also impacts customer experience. Studies show that an average of 63% of denied claims are recoverable, but hospitals pay a heavy price for it – $118 per claim – translating to about $9 BN a year in appeals-related administrative costs. This is where the transformative powers of Intelligent Automation can come to the aid of Providers.
Why legacy systems don’t cut it anymore
Despite the proliferation of automation technologies that can accelerate D&A management, nearly a third of the Healthcare Providers rely on manual resolution, as per a HIMSS survey. Legacy revenue cycle management systems require manual data input, compilation and segregation, increasing cycle time and turning the focus away from patient care to data management. Additionally, it also results in human errors (see Figure 1), leading to delayed patient appeals or complaints, negative experiences, compliance issues, and ultimately loss of reputation and revenue for hospitals.
The buck doesn’t stop here. With denials piling up regularly, the number of appeals also tends to climb – setting off a vicious cycle. The average 350-bed hospital saw denials leaping by 79% between 2011 and 2017, up from $3.9 million to $7 million.

Figure 1: Human errors in the D&A process
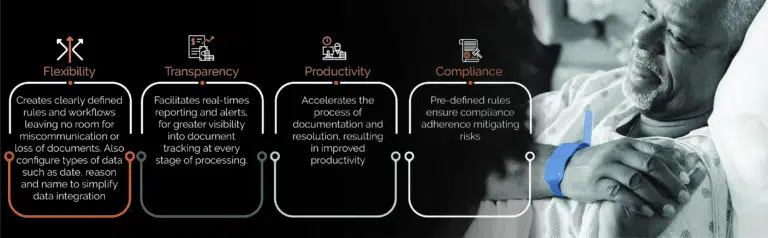
At the same time, Healthcare Providers are struggling to improve compliance, increase productivity, minimize penalties, increase visibility and transparency – all while lowering operational costs and enhancing the patient experience.
How Intelligent Automation can help
Intelligent Automation is the amalgamation of Robotic Process Automation (RPA) and Artificial Intelligence (AI). On the one hand, RPA automates rule-based repetitive tasks, helping healthcare organizations manage costs, reduce errors, and improve efficiency. On the other, AI helps extract relevant content using technologies such as Optical Character Recognition and combines it with intelligent workflows to accelerate the entire process.
A typical Healthcare Provider receives a high volume of denials. These claims rejections must be classified as a certain type and routed to the appropriate team to resolve. Classifying these denials is usually a manual process. Moreover, applying consistent human judgement to provide accurate sub-classifications – expedite, appeal or accept, etc. – is challenging.
The operations involved in handling denials and appeals – document management, business process management, and review and monitoring – lend themselves perfectly to Intelligent Automation. (see Figure 2).
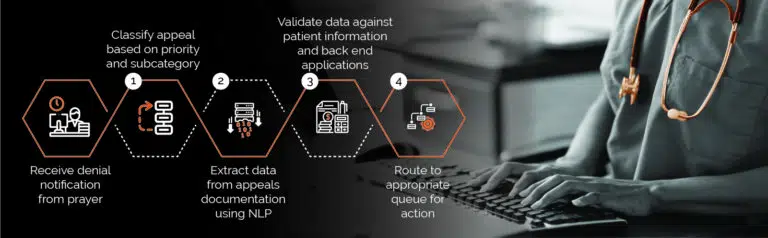
Intelligent Automation can replace steps 1-4 above, improving agility & scale.
Digitizing D&A management: Multi-pronged benefits
Intelligent Automation is proven to free up administrative capacity, while minimizing operational risks. It can extract and optimize accurate data from multiple systems and provide insights that help accelerate the process and elevate patient experience. Automated report generation and streamlined workflows further enhance the experience. It provides hospitals with the required flexibility, transparency, productivity, and compliance support.
Moving to a new paradigm
Even prior to the onset of the pandemic, Healthcare Providers recognized the importance of automation and were ratcheting up its adoption across the revenue cycle management function.
The global health crisis has further accelerated the need for automation to improve the patient experience while reducing operational costs. Applying a digital-first approach to D&A management will put Providers on the path to end-to-end digitization, impacting every aspect of the value chain – from boosting efficiencies and productivity to elevating patient experience and outcomes.
Further Reading: 5 benefits Healthcare Providers can reap by streamlining denial management through Intelligent Automation
How Firstsource can help Healthcare Providers stay ahead With Intelligent Automation
Firstsource’s Business Process Automation Services are designed to identify the root cause, assess impact of operational impediments, and recommend and implement automated solutions to streamline processes and create scale. We help leading Healthcare Providers implement Intelligent Automation, integrating applications and platforms for agility and performance.
Watch How Healthcare Providers can leverage Intelligent Automation
Firstsource partners with Healthcare Providers to enable Intelligent Automation of their processes by offering Automation as a Service (AaaS) across clinical and revenue management value chains, spanning the end-to-end patient journey as well as back-office administrative support. From automating core EHR functions, revenue cycle management, to automating processes such as Prior Authorization, patient scheduling, eligibility verification, and physician credentialing, our Intelligent Automation solutions positively impact revenue, patient experience, and employee satisfaction.
Download our eBook ‘Driving Impact at Scale with Intelligent Automation’ which serves as a complete implementation guide for Healthcare Providers.
Reference
- Philip Betbeze, Claims Appeals Cost Hospitals Up to $8.6B Annually, HealthLeaders, June 26, 2017
- Jacqueline LaPointe, 31% of Providers Still Use Manual Claims Denial Management, RevCycle Intelligence, July 5, 2016
- Kelly Gooch, “4 ways hospitals can lower claim denial rates,” Becker’s Hospital CFO Report, Jan. 5, 2018











