More value, in every moment
In the work you do, every interaction is valuable. There are no small jobs. No insignificant experiences. It’s why our intelligent back office is built to make it simpler for all stakeholders – your employees, members and providers — to work efficiently and optimize costs.
Together, we ensure you have the intelligent solutions and human-powered support to deliver exceptional experiences in every moment.

Pivot to Digital. Challenge the status quo
Upend traditional healthcare delivery with our Intelligent Automation solutions that integrate Robotic Process Automation (RPA) with Artificial Intelligence (AI) to drive unparalleled operational efficiencies, productivity and patient care.

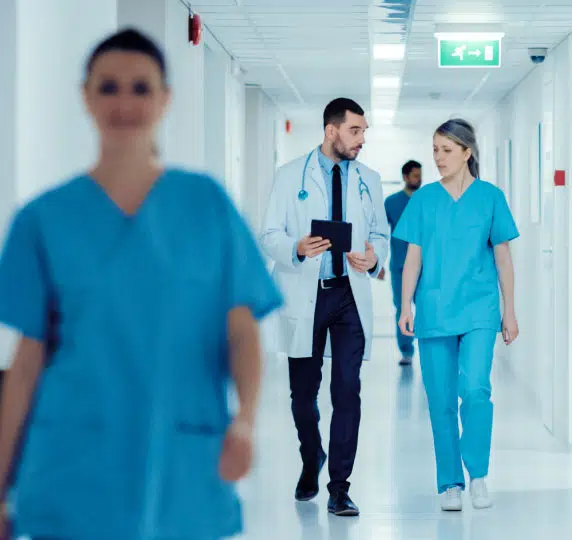
Holly Hans, Claims Vice President at CareSource
Bringing strategic clarity and deep industry perspective to CareSource — helping shape priorities, guide decisions, and power what’s next.