How Providers can enhance patient care by accelerating eligibility & insurance verification

2020 has been an unprecedented year for healthcare professionals and service providers. The global pandemic has put a substantial burden on the industry, which is already falling short of patient expectations, crippled with staff shortages and a growing financial crisis.
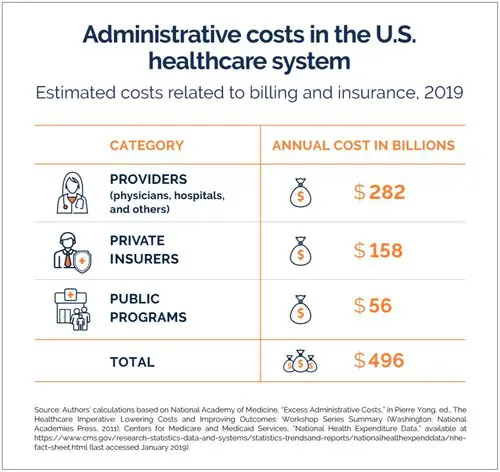
Amidst the existing resource constraints, administrative responsibilities further consume valuable time that can be devoted to patient care by Providers. According to the Center for American Progress, every year, Healthcare Payers and Providers in the US spend about $496 billion on billing and insurance-related costs alone.1 Given the impact of COVID-19, the costs are only going to escalate.
In this article, we would like to shed light on one of the biggest administrative challenges of US Healthcare Providers, namely eligibility and insurance verification; and explore ways in which Intelligent Automation can help improve outcomes.
Impact Of COVID-19 on eligibility & insurance verification Process
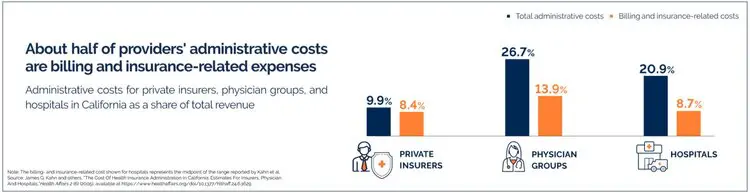
Do you know how excess administrative costs are burdening the US healthcare system?
Administrative processes encompassing heavy paperwork and documentation dealing with tons of data on insurance coverage, billing, procurement, and others form the backbone of healthcare systems. As per a recent study, in the US alone, the administrative costs of care account for 8% healthcare spending.2 And about half of Healthcare Providers’ administrative costs are billing and insurance-related expenses.1
When it comes to processing insurance claims, eligibility checks play a significant role in ensuring that patients are aware of their financial responsibility; and the claims submitted to payers for procedures meet their plan requirements. It involves going through every document and extracting information related to copays, coinsurance, deductibles, etc.
Though this is an extremely time-intensive process and prone to manual errors, it is vital to avoid claim resubmission, reduce demographic/eligibility related rejections/denials and follow up collection efforts leading to improved patient satisfaction. Incorrect or inaccurate insurance information often results in delayed payment or claim denials impacting the overall revenue for providers.

As per the 2019 Merritt Hawkins Physicians Inpatient/Outpatient Revenue Survey, elective orthopedic and cardiac surgical procedures were the most profitable for hospitals. However, since the onset of COVID-19, these procedures have taken a backseat, leading to a significant reduction in revenue. At the same time, patient satisfaction has hit a new low. Due to limited or lack of streamlined insurance counters in hospitals, issues related to patient medical insurances are on a continual rise.
This is where Intelligent Automation can help. To cope up with the increasing healthcare service demand and rising staff burnout, it is time to leverage Intelligent Automation to navigate through this crisis and transit to the new normal.
How can Intelligent Automation help streamline the insurance eligibility and verification process?
When the process of verifying patient insurance eligibility is automated, AI-powered bots help complete the verification in less than half the time taken by administrative staff. Leveraging digital intake with Natural Language Processing (NLP) along with RPA can help identify texts and numbers from any language or format and extract relevant information to make informed decisions.
It can verify every minute detail of the patient’s historical data such as mismatched financial information or customer details from the insurance policy. Applying AI/ML algorithms to this process can help further validate policy terms, renewal dates, and other hidden costs and conditions This minimizes delays and improves cycle time to streamline and speed up claims-related operations.
While Intelligent Automation takes care of the repetitive, rule-based tasks, it also helps mitigate staff burnouts and shortages. With mundane tasks managed by bots, the workforce is redirected to take up higher value-added, patient-centric strategic roles, such as improving case management, exception handling, which can help enhance patient care and experience.