AI-based solutions help identify and engage underserved members and populations to enable health plans to excel under new reward factor
In the current healthcare delivery environment, CMS Star Ratings have a direct impact on the financial success of Medicare Advantage and Part D prescription drug plans (MAPD) by influencing which plans members select.
However, the conversation surrounding Star Ratings has evolved beyond mere point accumulation. Increasingly, the focus is shifting towards health equity, equal access to high-quality healthcare for all populations, and outcomes across diverse populations, race, ethnicity, socioeconomic status. Therefore, from 2027 onwards, CMS is going to replace the existing reward factor with Health Equity Index (HEI) rewards. In this scenario qualified contracts will be eligible to receive between 0.1 to 0.4 additional points to the Star Ratings based on performance evaluation, with the objective to address disparities and improve care quality for socially at-risk beneficiaries.
The Business Case for an AI-First Approach to Improving Health Equity
It’s becoming more difficult for MAPD plans to increase their Star Ratings even as the Medicare Advantage marketplace becomes increasingly competitive. In 2024, Just over 40% of plans achieved four or more stars. Replacing the current reward factor with the HEI-based factor likely will make it more challenging for plans to boost their ratings. Under the HEI-based reward factor, CMS expects 75% of all 5-Star contracts to fall to 4.5-Stars—and lose the marketing and enrollment advantages that come with being a 5-Star plan. Further, estimates indicate about 60% of 4.5 Star contracts could drop to 4 Stars under HEI metrics.
In short, improving Star Ratings, or even simply preserving them, requires health plans to prepare for the impact of the HEI reward factor.
Fortunately, plans may now turn to a powerful array of generative AI and analytics tools to help them identify members and prospects with social risks, engage them with a combination of high tech and high touch tactics and improve their adherence for better outcomes. Below, we discuss how health plans can use AI-first strategies and incorporate generative AI tools to accomplish this task.
Defining an AI-First Strategy for Addressing Health Equity
An effective AI-first health equity strategy will use generative AI tools and data analysis across multiple channels to detect social risk factors, which range from socioeconomic issues, housing and food insecurity, transportation challenges, sexual orientation, and gender identity (SOGI) issues and race, ethnicity and language (REaL). This data is not always captured in electronic health records, with Z codes still underused.
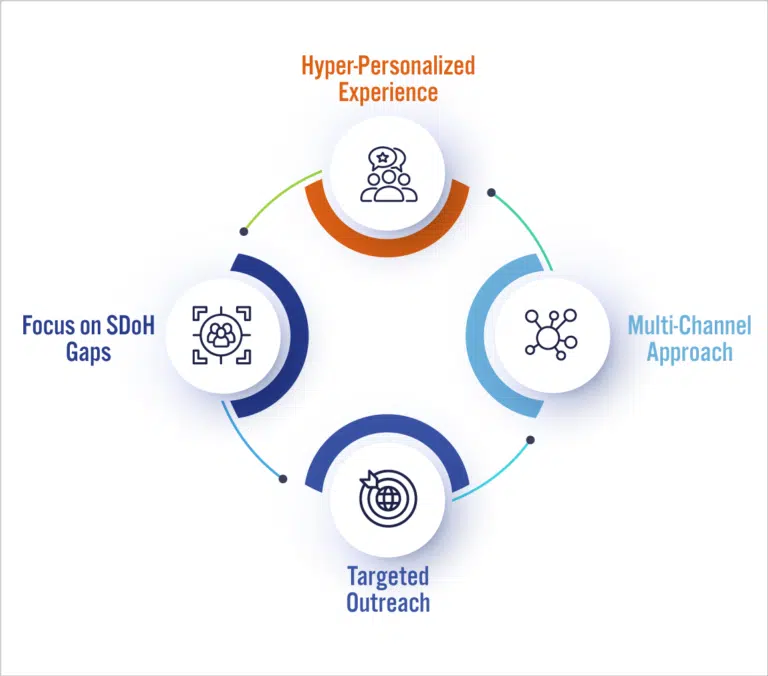
Much health equity data is highly sensitive and underserved individuals often are reluctant to disclose personal details without a high degree of trust and transparency. Plans may mitigate these concerns using generative AI tools and methods that deliver hyper-personalized experiences and engagement that clearly show the plan is addressing an individual’s unique needs.
Components of an AI-First Health Equity Strategy
Identification
Gen AI, a powerful tool, equips payers with insights into their population’s social risk factors. By analyzing call center conversations, GenAI LLM models can swiftly scan and summarize frequently discussed topics during or after the call. It can also identify patterns that indicate language barriers, cultural misunderstandings, or difficulties in navigating care pathways. Analytics tools use this data to delineate the characteristics of different member segments and their likely reactions to different communication channels and content. Understanding members’ characteristics enables plans to anticipate member sensitivities about their SDoH challenges. These valuable insights can then be used to initiate targeted interventions, such as providing multilingual support, addressing specific health concerns through educational materials, or coordinating community services to mitigate SDoH challenges.
Targeted digital outreach campaigns
AI enables health plans to create targeted digital outreach campaigns built on insights from Health Risk Assessment (HRA) surveys, risk adjustment HCC data, and identified underserved members. Combining this data with AI, plans can reach out to members with personalized follow-up surveys that fit the member’s context and are easily completed. Gen AI powered tools can even schedule primary care appointments during which AI agents can help physicians capture additional SDoH and SOGI information.
Personalized experiences and engagement
Gen AI can personalize onboarding experiences, remember member preferences and continuously assist members. Members calling into the regular phone line can be greeted by a Gen AI agent that understands the member’s context and is trained to accurately answer questions. From inquiries about insurance card delivery to selecting a primary care physician and plan coverage details, Gen AI seamlessly manages basic questions with intent identifiers running on speech-to-text translations and pulling up product benefits. These techniques will also help plans perform better on CMS measures such as ‘Getting Appointments and Care Quickly’, ‘Customer Service’, ‘Call Center’, ‘Foreign Language Interpreter and TTY Availability’, which are all weighted at 4x and can highly influence Star Ratings.
For a 65-year-old Hispanic individual facing language barriers, low confidence, and transportation challenges, Gen AI provides bilingual support, gentle nudges, appointment coordination, follow-up reminders, and connections to community resources, all in Spanish. This ensures clear communication, builds confidence, and addresses transportation issues, enhancing the member’s healthcare experience.
Adherence through multichannel outreach
Multichannel outreach tailored to members’ specific needs and preferences, including targeted emails, paper, text messages, web, microsites and outbound IVR calls, will gently nudge patients towards preventive screenings or medication adherence. Gen AI-powered interactions can provide 24/7 personalized support, answer member questions and even schedule appointments, including those with an impact on quality measures, such as mammograms.
Based on our experience, Visual IVR and conversational AI channels have proven most effective for individuals aged 65 and above. Millennials prefer portals and self-service Gen AI-based apps. Research also shows Medicaid members are typically comfortable with digital tools.
In our work with one client, we have developed proactive, personalized appointment confirmations and reminders resulting in more than 60% increase in engagement rate and an 85% increase in conversion rate. For another client, we implemented a hyper-personalized visit adherence solution delivered through an omnichannel communication platform, improving member experience ratings by more than 30% and significantly reduced no-shows and late cancellations.
Multichannel hyper personal approaches powered by Gen AI can also indicate when an at-risk member requires a high-touch experience. For example, an elderly member called into the help line of one of our clients because she did not understand the educational materials mailed to her. An AI agent was able to quickly recognize that the member did not understand much English and routed her to a service representative who worked closely with her to explain the information. The representative texted a link that took the member to an AI-powered microsite, and during the call guided the member to navigate the microsite with our agent assist capability. The microsite adapted its presentation to the member’s language and content needs, reinforcing the highly personal treatment from the representative.
Digital reminders and telehealth consultations for medication management demonstrably increase medication adherence, directly impacting chronic disease management HEDIS measures and, therefore, Star Ratings. (Source: Journal of Medical Internet Research, 2022)
Steps to Take Now
The impact of the Health Equity Index (HEI) on Star Ratings presents both a challenge and an opportunity for health plans. Using data from the 2024 and 2025 plan years, the new HEI reward factor will be reflected in 2027 Star Ratings.
Here are some immediate steps to take to avoid losing Stars:
- Calculate the potential impact of the HEI reward factor on current ratings and examine how well your organization addresses socially at-risk populations, including underserved members and dual eligibles.
- Assess current technological capabilities, inventorying dependencies on legacy tools and processes and whether the flexibility exists to implement Gen AI or AI-like functions.
- Evaluate service providers’ abilities and experience in launching and managing multifaceted AI-first strategies to improving health equity.
By addressing these areas, plans can comply with new regulatory requirements and improve their service delivery and member satisfaction, positioning themselves to enhance their Star Ratings as healthcare equity standards evolve.
For more information on how artificial intelligence can be leveraged to address the impact of the CMS Health Equity Index on Star Ratings, please contact Deepan Vashi, EVP – Healthcare Payer Practice and Solutions Lead, Solutions Architecture, Firstsource, or contributing authors, Priyanka Grover, AVP – Firstsource Health Plans and Healthcare Services and Nikita Agrawal, Assistant Manager – Firstsource Health Plans and Healthcare Services.