While AI has been at work in healthcare in many forms, such as predictive analytics and image recognition, generative AI is capturing the most attention right now. Generative AI’s ability to quickly synthesize original content based on literally thousands of sources makes it especially attractive in healthcare, with the industry’s ever-growing troves of administrative and clinical data. Gen-AI models such as ChatGPT, BARD, Claude, John Snow Lab, etc. have been built on large language models (LLMS). An LLM learns a vast quantity of unstructured information. Given a prompt, a Gen-AI model draws on the patterns it has learned within an LLM to generate original content, including text, images, music, configuration, and even software code. By providing feedback about the accuracy or appropriateness of the results to machine learning algorithms built into the model, generative AI gets better at how it responds to prompts and assembles content.
Where Gen-AI Works for Healthcare Payers
Gen-AI will deliver real business results; for many use cases, it will bring new capabilities to old problems, such as how to summarize findings in literally millions of medical records. Gen-AI also will be layered into health plans’ existing automation and “narrow” AI and Machine Learning (ML) solutions for greater performance and returns. The key to early wins with Gen-AI is finding the right cases.
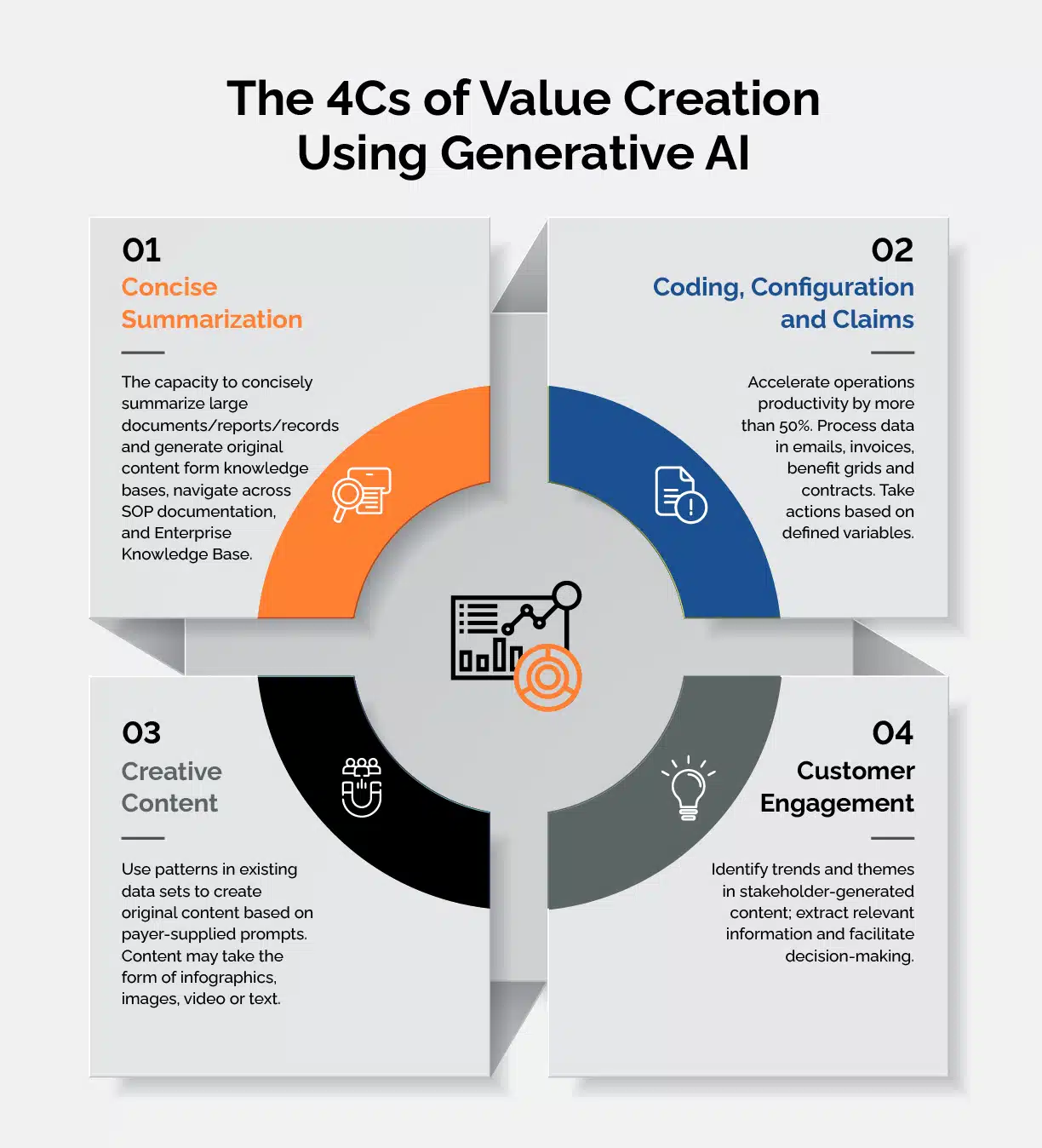
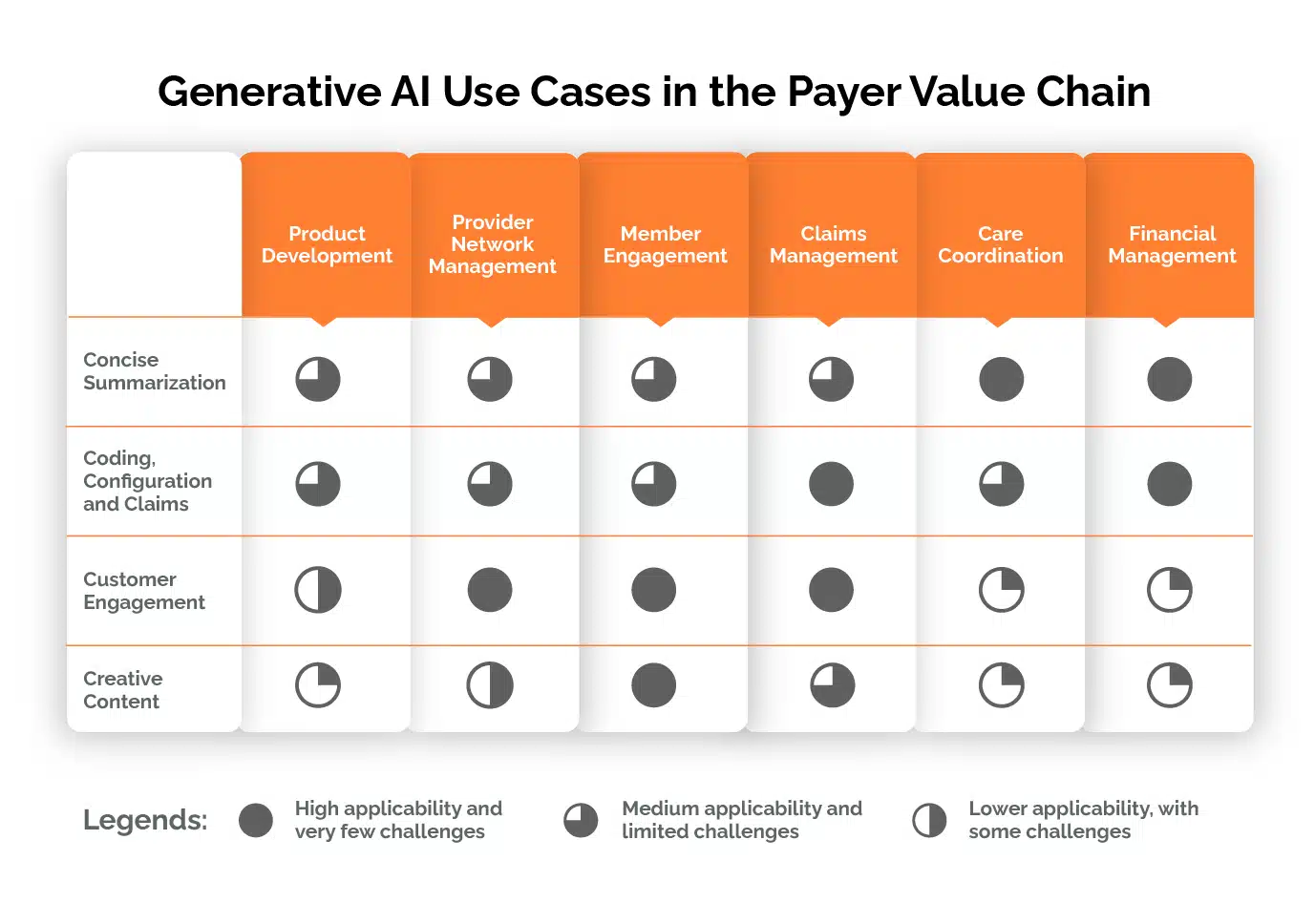
The consulting firm McKinsey has mapped generative AI value casesto four broad areas: customer engagement; concise expertise; coding; and creative content. With a nod to that framework, we’ve adapted it to the payer value chain.. Our goal is to give payers more insight into how they can use generative AI in practical, productivity-enhancing ways. Piloting applications and testing use cases is the best way to understand and unlock the potential of this technology.
Concise Summarization
Develop concise standard operating procedures (SOPs) and desk-level procedures, generate summaries of large documents and records, extract diagnoses and symptoms from medical charts; and make all claims, attachments, correspondence, and appeals received from paper and fax channels searchable documents.
Coding, Configuration and Claims
Augment existing platform and operator abilities in processing claims, managing benefits and contact configuration loading, matching providers and prior authorizations with claims, and blending Gen-AI and Predictive-AI for COB
Customer Engagement
Streamline benefits and claims status inquiries with Gen-AI, customize and recommend benefits plans, provide personalized next best steps to member and provider services associates, agents, and brokers, and improve services with continuous feedback based on 100% of contact center interactions – calls, chat, email.
Creative Content
Develop creative training material and process simulations from existing SOPs. Support personalized member benefit explanations, personalize member/provider education materials, marketing communications, advertisement copy, and investor materials.
Concise Summarization: Gen-AI models are designed to create new content based on language and logic patterns in the LLMs on which they have been trained. That new content can be concise summaries of patterns or specific data elements in literally millions of files and records. Additional training on specialized LLMs and industry and company-specific data sets finetunes generative AI’s abilities in this area.
- Prior Authorizations. Gen-AI can take over the time-consuming, low-value but necessary manual tasks associated with prior authorization, such as information searching, collating, and cross-checking structured and unstructured documents. A Gen-AI application organizes and/or summarizes information from (EHRs), email, policies, medical protocols, and various other sources. These capabilities will be even more critical as health plans eliminate prior authorization for many common procedural codes. The remaining codes requiring prior authorization are likely to be more complex cases. Gen-AI will search and summarize documentation, such as medical summaries and clinical papers, to support clinical decision-making.
- Medicare Advantage risk adjustment reviews. After training on appropriate datasets and assimilating coding guidelines, Gen-AI can swiftly review thousands of claims to identify medical conditions, procedures and details not captured in claims data that signal the need for an additional or adjusted code. This greatly reduces the manual labor involved in risk adjustment reviews, mitigates the potential for human error, and improves the accuracy of risk assessment computations. Extensive, accurate data can help payers substantiate their population risk scores for appropriate compensation and reduce the regulatory risk.
Claims and Configuration operations: In streamlining claims and configuration operations, Gen-AI often can be layered into existing automation and narrow AI solutions to enhance performance by augmenting their capabilities. Using Gen-AI in these contexts can drive higher returns from health existing operations investments.
- Faster claims adjudication and accurate reimbursement. Gen-AI-equipped engines act as co-pilots alongside core administrative platforms and assist adjudicators in quickly dealing with edit codes and claims that can’t be auto-adjudicated. By digesting data about claims, benefits, medical guidelines, and standard operating procedures, Gen-AI can provide adjudicators with relevant SOP data and summaries of services rendered. Gen-AI models also can create personalized denial letters, consolidate denial codes, highlight relevant denial reasons, and contextualize and provide the next steps for denial management.
- Benefits and provider contract configuration. The benefit grids and provider contracts have traditionally been loaded manually by configuration experts. A Gen-AI Config Copilot will assimilate necessary information into a template for a quick human-in-the-loop (HITL) review and the configuration template is ready to be loaded by bots, improving accuracy and reducing the timeline from hours to minutes.
- Fraud detection. Health plans may create more comprehensive fraud detection systems by combining Gen-AI’s ability to simulate normal behavior with narrow AI’s rule-based machine learning models. The Gen-AI model establishes a baseline of expected behavior, while narrow AI models identify deviations from the baseline. Gen-AI algorithms digest extensive data sets, identify anomalies and patterns, and recognize known fraud schemes, empowering SIUs to intervene early and minimize losses. Real-time monitoring of claims content, behavioral analysis, and risk scoring are some of the key capabilities of Gen-AI to apply to fraud prevention efforts.
- Smart Mailbox. Efficient email triaging plays a pivotal role in ensuring that healthcare payers can respond faster and deliver seamless services to their providers and members. By harnessing the power of advanced Natural Language Processing (NLP) models, payers can now automate and streamline the intricate manual process of reading emails to identify multiple intents and respond to them by collating information across various systems and departments.
For example, from onboarding and credentialing providers to managing provider data updates, contract negotiations, and beyond, Gen-AI systems can analyze the content of incoming emails, understand the intents and accurately route them to the appropriate work queues, avoiding misroutes and ensuring delivery to the right teams. The same Gen-AI can help agents respond to service requests with humanized auto-generated responses. This not only accelerates response times but also enhances the accuracy of handling critical tasks, ultimately leading to improved provider satisfaction and operational efficiency in the healthcare payer ecosystem.
Customer engagement: Payers can tap Gen-AI’s facility with natural language and its ability to synthesize new content to deliver better service to all stakeholders.
- Better stakeholder services and engagement. Gen-AI in combination with other tools can greatly speed responses to stakeholder queries, such as eligibility, benefits, and claims. With the right training, Gen-AI can recognize keywords and match them to their clinical synonyms and either provide responses or prompt human agents to handle the inquiry.
Gen-AI also can review the content of 100% of contact center interactionsvs. the 2%-3% typical of the usual quality audits. Health planscan configure the variables for the Gen-AI to highlight necessary improvements. When done in real time, the AI can provide feedback and relevant information even as a customer service representative is managing an interaction. Gen-AI can also summarize the audit data for use in training and continuous improvement programs. - Empower brokers and agents with member insights. Empower sales agents with real-time insights and predictive analytics. By reviewing customer data, AI algorithms can identify patterns and correlate these with known health risks and potential medical needs. Armed with this knowledge, sales agents can provide personalized recommendations and guidance, so members’ insurance plans offer coverage that’s appropriate for their unique needs.
A Gen-AI model continuously monitors data and prompts identified changes in members’ health or circumstances alerting the sales agent to these with suggestions about whether to update or modify insurance coverage. This proactive approach helps ensure members have the most relevant coverage for their evolving needs resulting in higher member satisfaction and loyalty.
Creative content. Gen-AI is set apart from narrow AI by its ability to generate original content. While content such as advertising copy and marketing material falls under the “creative” category, Gen-AI can also assemble much more sophisticated content to help payers develop new business models and improve member outcomes.
- Engaging training material and simulators. Gen-AI can leverage the existing SOPs and content to create training material, quizzes, simulations, and case studies. An Instructional Design Copilot will help develop modular training material 50% faster resulting in quick ramps.
- Customized benefits plan creation. Gen-AI’s ability to swiftly build new content will revolutionize how health insurance is sold. Using clinical, demographic, and benefits data, Gen-AI could understand members’ and prospects’ specific needs and risk profiles. Then AI algorithms can generate customized benefits that align with member requirements. Payers could then build personalized plans offering these benefits.
Individualized care management plans. Gen-AI can help enrich care managers’ interactions with members by producing personalized education materials and draft care plans based on best practices and an individual member’s demographic, social determinant of health, and clinical data. Care managers would review the customized care plan and finetune it as necessary.
The value of working with Gen-AI today
Gen-AI shows great promise for enabling healthcare organizations to streamline their operations. But it is not plug-and-play technology, yet. In many instances, a Gen-AI model must be coupled with other machine learning algorithms, platforms, applications, and analytical tools to deliver game-changing results. Healthcare organizations must also address AI’s ethical issues. These include protecting members’ personal health information; transparency, i.e., understanding how a Gen-AI model arrived at its conclusions; avoiding bias in data sets so the AI model doesn’t perpetuate them; and quality control. That last point acknowledges the fact that Gen-AI may return incorrect or incomplete information in response to a prompt. A Human-in-the-loop approach will ensure its results for accuracy.
That’s one reason why many payers will find the most efficient way forward with Gen-AI is to work with a payer operations partner who has built a best-in-class AI tech ecosystem. By taking this approach, a payer can focus on its business objectives while its lead partner coordinates the design and deployment of Gen-AI pilots. It also helps payers avoid the time and significant expense of developing a comprehensive internal AI expertise. Instead, health plan leaders can focus on deployment, change management, business outcomes and appreciate its strengths and challenges.
Getting started now, despite gaps in Gen-AI abilities, is key. Payers who experiment with proofs of concept and pilot programs will gain a first-hand understanding of what’s needed to drive value from Gen-AI. Also, instead of taking enterprise data to the centrally managed, cloud-hosted Gen-AI models, from a privacy and security perspective, it is more practical to bring closed LLM models to the enterprise data. That knowledge will be a solid foundation for increasing the sophistication of use cases and deriving advantages from Gen-AI capabilities, from driving operational efficiency to improving outcomes and delivering greater value to stakeholders.
For additional information or questions on how Firstsource can help your organization adopt AI, please reach out to contributing authors Deepan Vashi, EVP and Head of Solutions for Firstsource Health Plans and Healthcare Services; Priyanka Grover, AVPFirstsource Health Plans and Healthcare Services; and Anushka Saxena, Firstsource Health Plans and Healthcare Services.










