Main Navigation New
-
What We Do
What We Do
We provide transformational solutions across the customer lifecycle in Healthcare, Banking, and Communications. Our specialized teams use advanced technology and data analytics to address clients' key challenges and deliver future-focused outcomes.Type 01Firstsource recognized as a Global Leader in Generative AI Services in ISG Provider Lens® 2025
Learn More -
Who We Are
Who We Are
Firstsource, part of the RP-Sanjiv Goenka Group, is a global business process management partner with a strong presence across the globe, supporting Fortune 500 and FTSE 100 companies.Know MoreType 02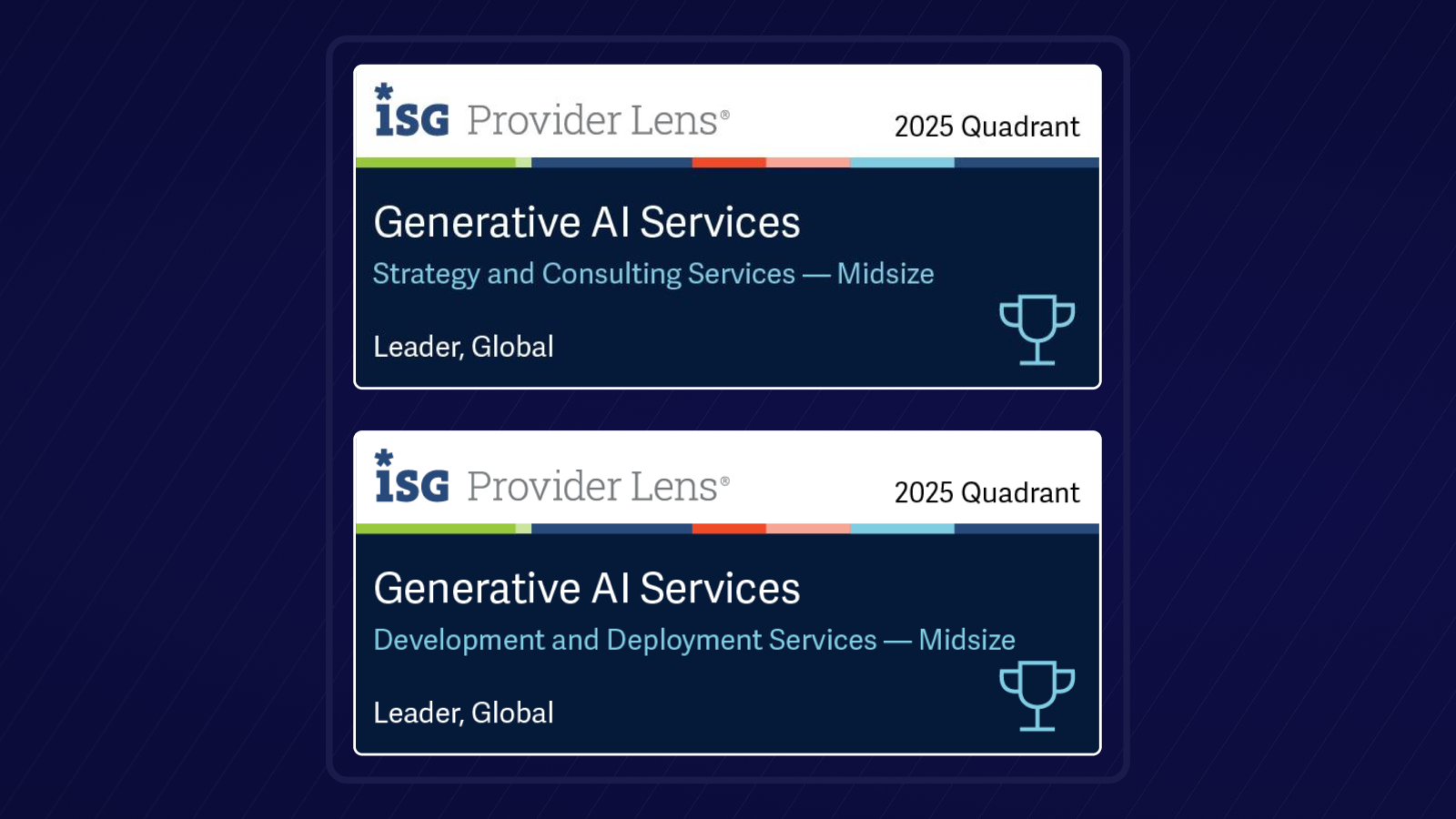
Firstsource recognized as a Global Leader in Generative AI Services in ISG Provider Lens® 2025
Learn MoreFirstsource Brands


-
Insights
Insights
Explore our case studies, blogs, ebooks, and podcasts for expert insights and actionable strategiesType 01What's trending?
Solving for Efficiency Inside a Media Giant's CX Transformation with Firstsource
Learn More -
Investors
Investors
Find financial reports, company performance metrics, and strategic insights. -
Newsroom
WHAT’S TRENDING?No Right Sidebar
-
Careers
Careers
Big ideas. Bigger dreams. Engaging work. Empowering culture. Learning opportunities.Know MoreType 04 - UnBPO™
Mobile main menu
mobile-main-menu
- What We Do
- Who We Are
- Insights
- Investors
- Newsroom
- Careers
- UnBPO™






