Generative AI is ready to transform health plan operating and business models
Much AI technology is now a commodity. No one needs to be an expert to use it. For health plans, that means it’s time to begin asking how and where to apply AI to operations and business models right now for real impact.
AI is a natural fit in multiple functions across the health plan value chain. Generative AI (GenAI) is trained to understand language and context and to create original, unscripted responses. Those capabilities mean GenAI is delivering real value today in claims operations, the contact center, in quality assurance, training and more. AI tools can solve perennial pain points, make employees more productive and help plans deliver better member and provider experiences. In the following, we look at AI’s core benefits and review just a few real-world use cases through which health plans are achieving measurable results with AI deployments today.
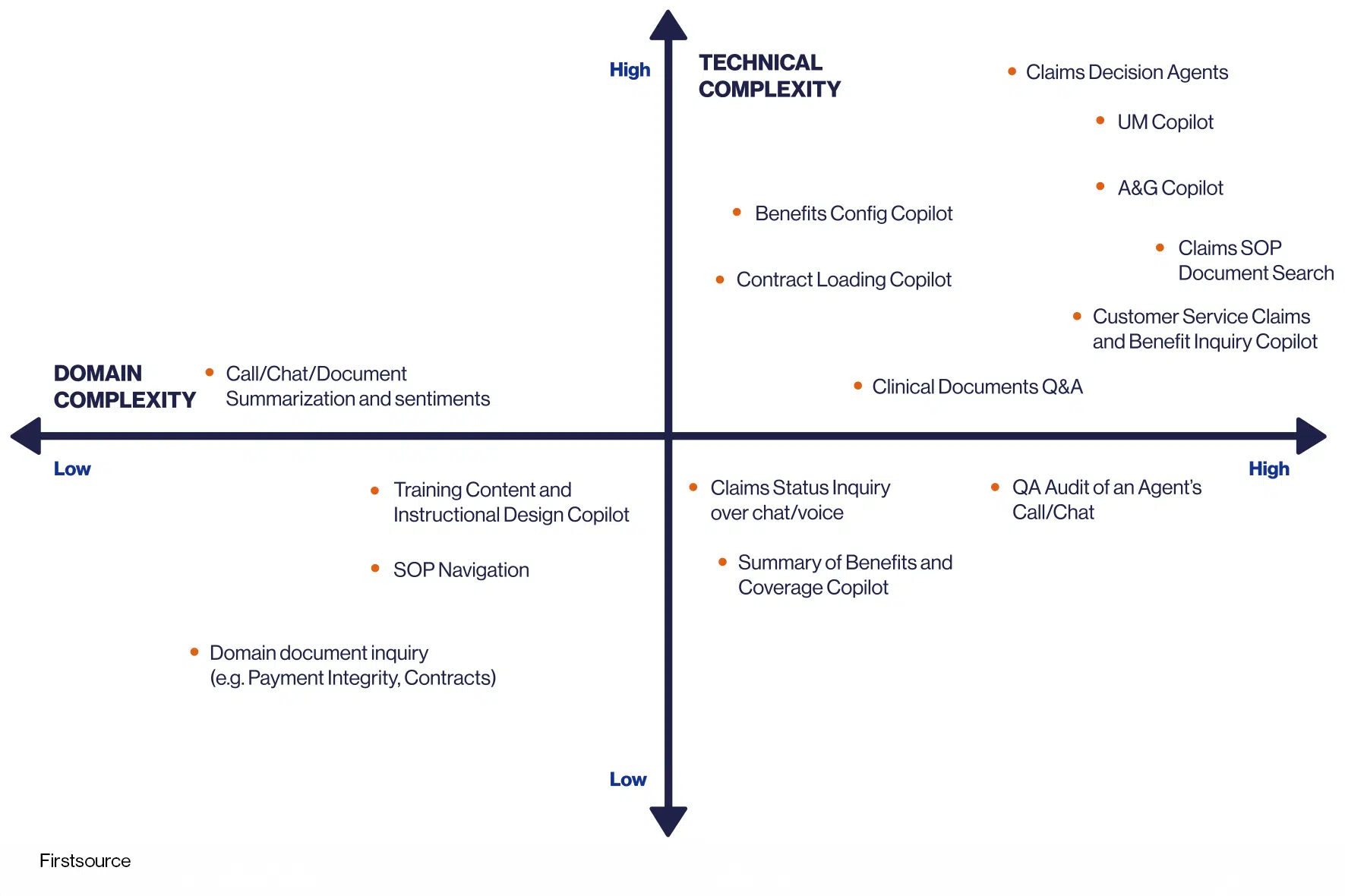
Al can deliver new performance throughout the payer value chain. The more complex the area of expertise, the greater the value Al will unlock for positions such as nurses, physicians and experienced professionals in prior authorization, adjudication and A&G.
AI Attributes Redefine Payer Business and Operations Best Practices
Operational efficiencies, clinical workflow support, improved member and provider experience, audit and compliance precision and intelligent content generation are among the key AI attributes that create value fast. Here’s a look at how a few of our clients are transforming their operations and business models with them.
Enhanced Operational Efficiency
Gen AI accelerates content extraction from emails, claims, contracts, medical records and more. This capability minimizes the need for staff to look up information, expedites service processes and increases opportunities for automation. These efficiencies can net considerable time and cost savings while improving services.
Communications: One of our clients, a top four health plan, is saving $5 million annually with our gen AI Smart Mailbox co-pilot. The client had more than 200 operations team members monitoring more than 80 email inboxes to read and route messages from members and providers. Our AI co-pilot now manages these inboxes. When an email arrives, such as a notification that an individual provider is leaving a plan’s network, the AI co-pilot reads the message, identifies the intent, i.e., that the physician listing should be removed, then creates a ticket within the plan’s customer relationship management (CRM) system to take that action. This is all achieved without manual intervention. The co-pilot can tackle multiple emails per minute, eradicating email backlogs.
When an email’s intent is unclear, the AI co-pilot routes it to the provider operations team, which now has the time to review and respond to complicated communications.
Claims Auto-adjudication: Another client is using our AI co-pilot to improve auto-adjudication rates and accuracy. For each claim, the co-pilot can identify the provider contract, the applicable health policy and benefits. Then it can calculate the allowed amount, compare that to the billed amount and adjudicate the claim -- all without manual intervention.
AI claims adjudication decision agents and copilots can predict and resolve potential pended claims during adjudication; make intelligent real-time claim edits; use member life events and claims data to predict potential COB in real-time; flag potential appeals and grievances claims; and check for over and under payments.
- Process Discovery and Automation: A leading national payer used our process mining to identify $25 million in potential savings in core platform operations by addressing issues with prior authorization, external pricing, external payment integrity edits, provider maintenance edits, and claims adjustments. AI-driven process mining can review all the steps that go into a process, detecting and reconstructing workflows, and visualizing those processes in real time. That transparent, objective view into current processes helps identify real performance issues, bottlenecks and friction points so all can be improved.
Optimized Clinical workflows
Gen AI autonomous agents evaluate clinical documents, ensuring personalized care plans and facilitating accurate medical necessity reviews with evidence-based criteria. Multiple AI agents can work together across the payer value chain to exchange information and act based on business rules. These agents and “agentic workflows” allow payers to streamline data-intensive processes.
- Prior authorization and appeals. Another of our clients is saving substantial time and 40% cost using our communication hub and copilots for appeals, correspondence and prior authorization. The AI co-pilot orchestrates multiple skills or AI agents to review and validate the information and triage incoming appeals and prior authorization requests. The co-pilot validates the request against the member and provider records, members’ benefit plans, payer guidelines and SOPs. It summarizes medical notes and presents information to the associate. If additional supporting information is required, the co-pilot generates an appropriate letter to the provider. The co-pilot routes complex requests to human agents; otherwise, it generates and transmits letters to the provider. Our client’s clinicians spend 46% less time reviewing authorizations and meet CMS requirements for prior auths and appeals.
Precision in Audit and Compliance
Gen AI agents scrutinize human associate interactions, ensuring adherence to quality standards, regulations and suggesting improvements in a non-intrusive way.
- Operations co-pilot. A large health plan ensures its claims adjudication team follows standard operating procedures (SOP) execution using our AI copilot. When a complex claim needs to be adjudicated, our AI agent reviews it in seconds and highlights its many line items, including any potentially incorrect procedural or diagnostic codes. The AI agent then provides the adjudicator with a URL to the precise payer procedures and steps in the SOP the adjudicator must follow to accurately process the claim. This process eliminates the five to seven minutes usually needed to research the claims scenario against the SOP steps, so now the adjudicators can take just two to three minutes per claim instead of ten. Further, the audit trail shows exactly what SOP applied to the claim.
- Contact center co-pilot. AI can identify the root causes behind calls from plan members or providers so plans can correct these. For calls that are not preventable, AI chatbots can respond to a variety of questions, including inquiries about benefits, claims status, and prior authorizations. AI co-pilots can assist human agents by suggesting next-best actions based on their near-instant analysis of a caller’s sentiment. During a call, the co-pilot can anticipate and deliver the data the agent will need to satisfy the caller, so the agent need not toggle between screens and applications. When calls are complete, AI co-pilot may review them, both for its own training and to identify where to improve the quality of member interactions.
Intelligent Content Design and Summarization
GenAI copilots enable faster time to competency for employees and customer service agents by personalizing training content, expediting content creation, distilling complex benefits data into concise summaries and enabling training simulations with an AI-coach.
Training. A leading national health plan we worked with had been told it would take about two months to create eLearning training material about a specific operating procedure. We developed a proof of concept in which an AI co-pilot turned written content into a multimedia, gamified training course with videos in one week and we produced the trainer instructions in just one day.
In a few minutes, the AI co-pilot read and summarized the key points of a 40-page document detailing the operating procedure. With guidance from the health plan on the essential training objectives, the co-pilot converted the content into training modules. The co-pilot developed slide decks, gamification elements and storyboards for videos – all in one day. We took another four days to review and verify the content. Using a plugin to a text-to-image generative AI tool, our co-pilot produced a training video with a single click. The bottom line: Our client had a robust training solution in about a week vs. two months.
Collaborative AI Agents
Multiple AI copilots across the value chain are working together and coordinating actions in an agentic workflow. Copilots in an agentic workflow for enrollment, prior authorization, medical records, claims, appeals and grievances and correspondence share data and follow complementary business rules. We helped a major national plan deploy AI co-pilots to work in tandem from its mailroom to provider data management to claims. For example, we are implementing a claims decision agent/co-pilot, correspondence, appeals and prior auth workflow that draws on several agentic workflows. The agentic flow verifies member data on a claim is accurate; checks edit codes and corrects; then evaluates whether the claim will adjudicate successfully. If the co-pilot has low confidence in a claim’s accuracy, it will route the claim to a human claims examiner for review.
Coordinated processes like agentic workflows enable AI to be increasingly practical throughout the payer value chain. A health plan’s employees likely have already used GenAI tools and have ideas about which processes and procedures AI could streamline. In addition, health plans should collaborate with service providers that have expertise in healthcare and AI. Together, and with AI co-pilots and agentic workflows, health plans will get proven, practical answers to the question, “How can we improve our operations with AI?”
For more information please contact Anup Panthaloor, EVP – Health Plans and Health Services or Deepan Vashi, EVP – Healthcare Payer Practice and Solutions Lead, Solutions Architecture, Firstsource. Visit Firstsource relAI to read about our suite of AI led platforms, solutions and offerings. Learn how we’re empowering businesses of all sizes to seamlessly integrate digital technology and AI into their operations to enable new levels of efficiency, innovation, and competitive advantage.










