We are pleased to share this blog authored by guest contributors, Ankur Verma, Vice President, Everest Group, and Vivek Kumar, Practice Director, Everest Group.
“Imagine a major regional health plan reducing administrative expenses by 30% and slashing technology debt by half in the process. Picture another health plan adding a new marketplace line of business in record time, tripling enrollments, and mitigating membership losses due to Medicaid redetermination.”
These transformative outcomes are not mere aspirations, but real results achieved through Business Process as a Service (BPaaS) solutions. As the health insurance landscape evolves, BPaaS offers a lifeline to payers navigating legacy systems and outdated operational models. (Figure 1)
By delivering faster turnarounds, enhanced flexibility, and measurable growth, BPaaS empowers healthcare payers to meet growing demands, manage regulatory complexities, and achieve operational excellence.
Below we explore the transformative journey of BPaaS, its impact on payer operations, and strategic guidance for industry leaders aiming to achieve groundbreaking results.
BPaaS in Practice - Transforming Payer Operations
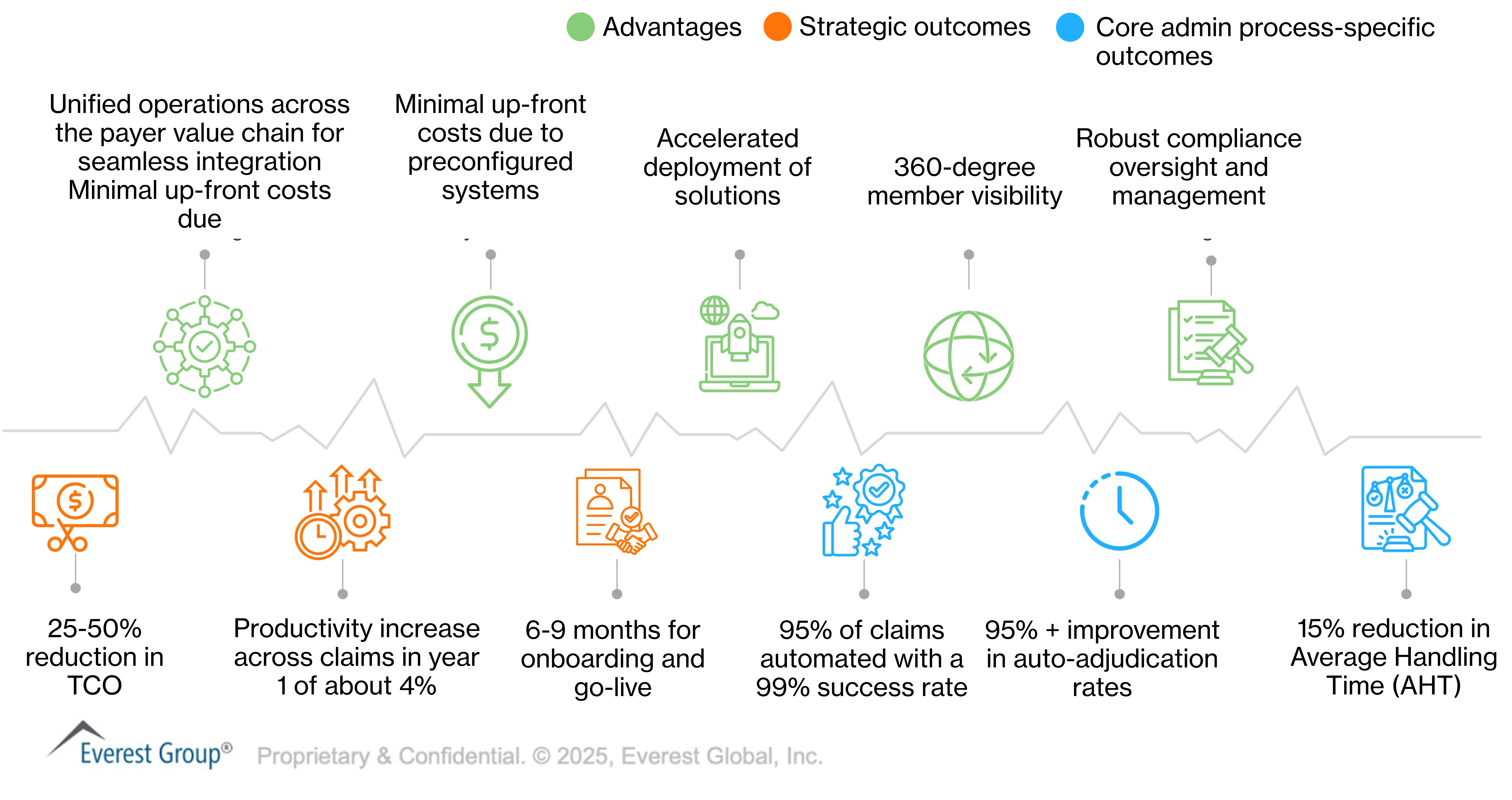
Figure 1
The evolution of BPaaS: From outdated to dynamic (the new GenAI powered BPaaS)
Over the past decade, BPaaS has transformed from a basic service model into a dynamic solution driven by five foundational pillars:
- Central Platform: Systems of engagement or record
- Integrated Services: Unified, end-to-end process management
- Cloud Deployment: Scalable, secure platforms reducing infrastructure dependencies
- Pay-As-You-Go Models: Flexible, cost-effective options tailored to organizational needs
- Scope: End-to-end BPaaS, line of business BPaaS and functional BPaaS
Today, technologies like Agentic AI, process mining, pre-configured tools, and Generative AI (GenAI) are reshaping the BPaaS landscape. In healthcare, these innovations enable seamless digital experiences, efficient onboarding, and enhanced auto-adjudication, positioning BPaaS as an indispensable tool for operational optimization.
AI-enabled tool & technologies redefining operational excellence
For healthcare CXOs, seamless digital experiences, efficient onboarding processes, and enhanced auto-adjudication are no longer optional — they are critical to maintaining competitiveness and operational efficiency.
Below, we explore how these technologies are revolutionizing BPaaS, positioning it as a key enabler for optimizing payer operations and making it “GenAI super-powered BPaaS”. (Figure 2)
GenAl powered super BPaaS
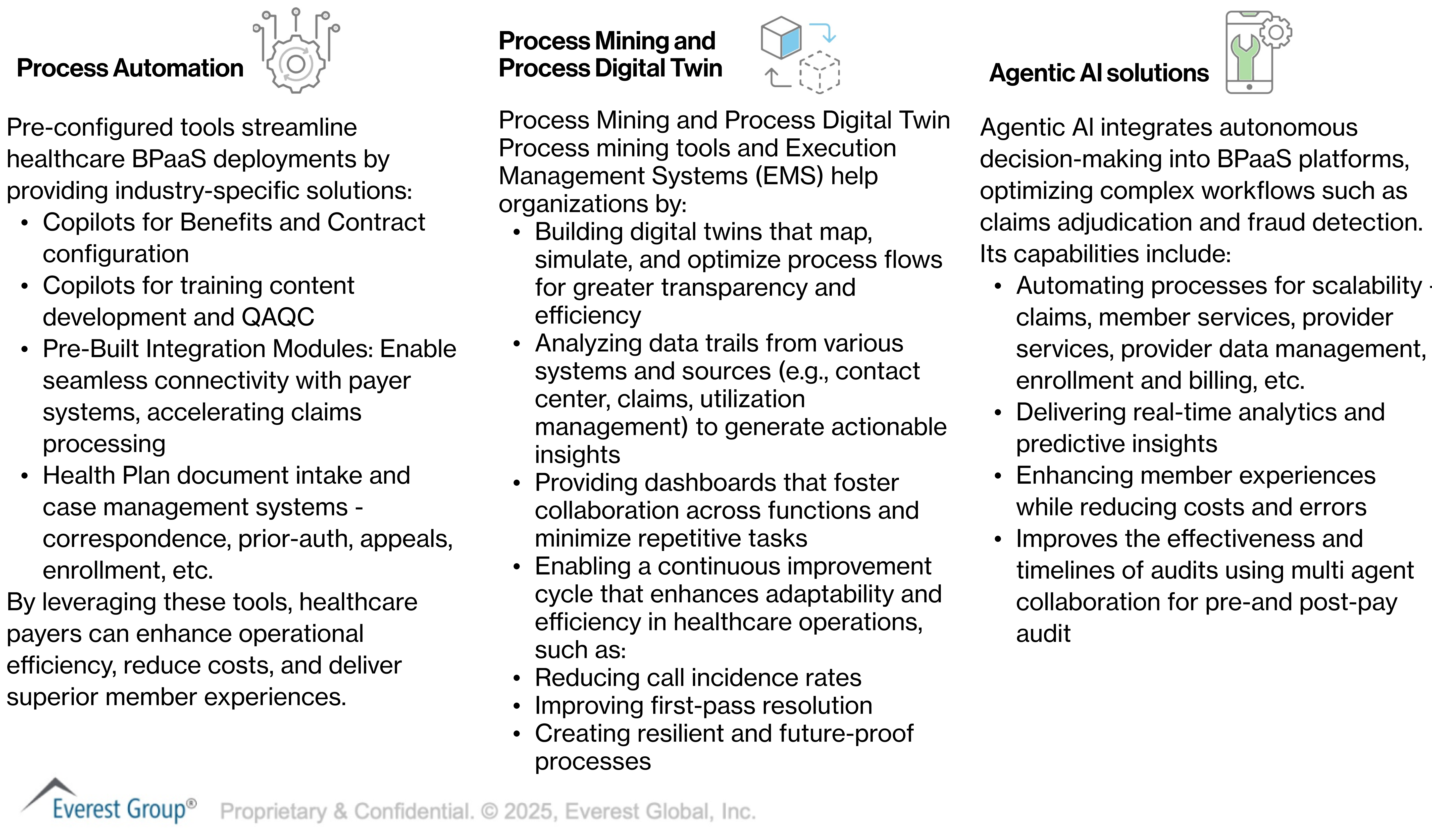
Figure 2
Evaluating BPaaS: What helps achieve high performance for CXOs
When CXOs consider implementing a BPaaS solution for claims, member services, or other operations, it is crucial for them to understand the key differentiators of a high-performance BPaaS, compared to traditional BPaaS or the absence of BPaaS altogether. The schematic below provides a comprehensive list to guide CXOs in evaluating and selecting the right BPaaS solution when the time comes for implementation. (Figure 3)
Evaluating BPaaS: A checklist for CXOs
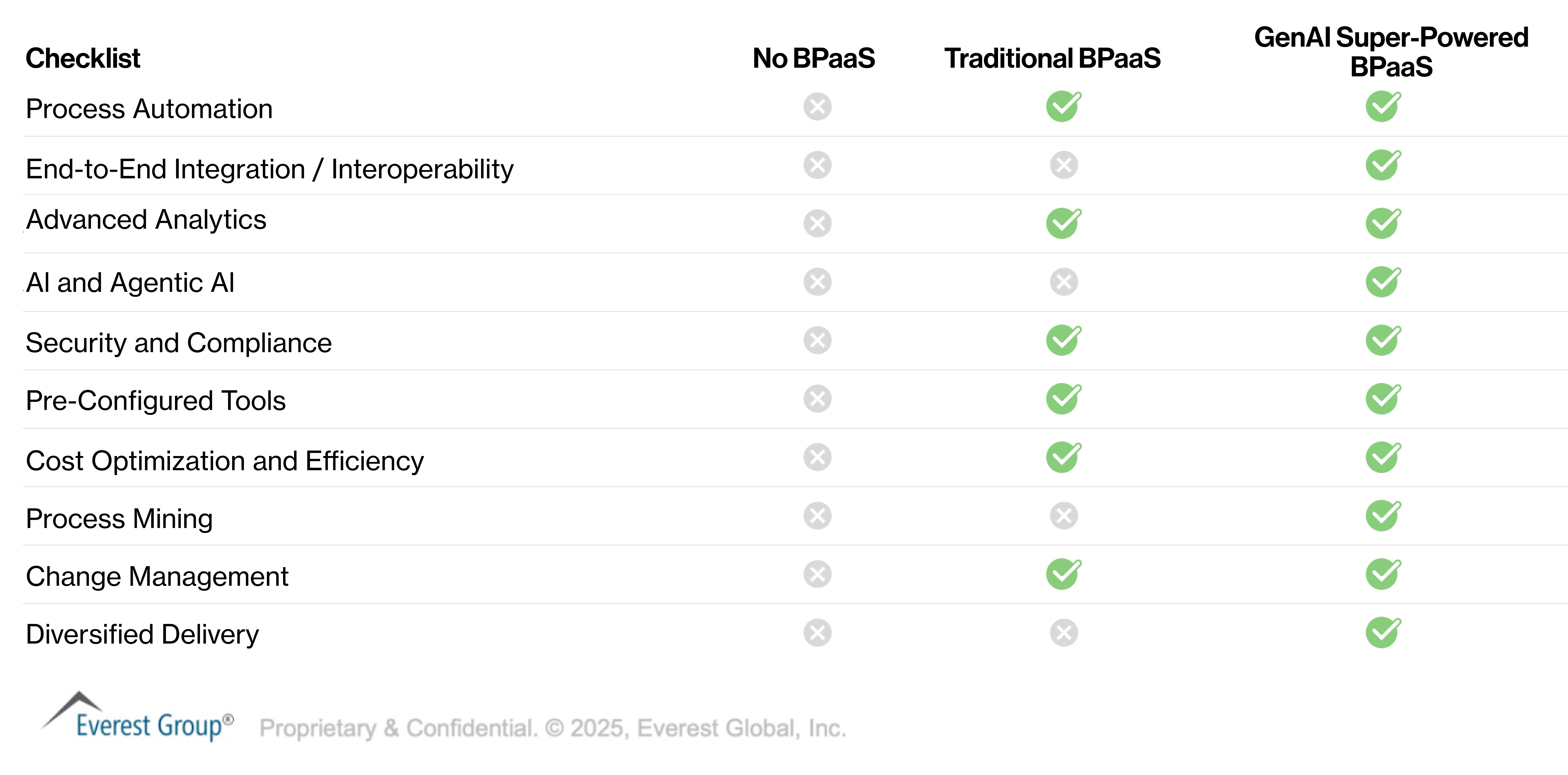
Figure 3
BPaaS Blueprint: Charting Your Course to Success and Seamless Implementation
Designing a BPaaS blueprint requires a structured approach that balances operational efficiency with strategic alignment. The following steps outline the key actions CXOs should take to develop a comprehensive BPaaS strategy, laying the groundwork for a successful implementation.
1. Assess Needs
- Map workflows (e.g., claims, onboarding) and identify inefficiencies.
- Set targeted goals like faster processing, cost reduction, or improved engagement.
2. Select Technology Partners and Create Security Roadmap
- Choose vendors with healthcare expertise, robust partner eco-system and scalable, compliant solutions.
- Ensure comprehensive interoperability with existing systems and EHRs.
- Implement encryption, access controls, and compliance (e.g., HIPAA).
- Use secure cloud infrastructure for scalability and agility.
3. Implement Core BPaaS Components
- Automate processes (claims validation, communications).
- Integrate AI for analytics and adaptive workflows.
- Use pre-configured tools for payer-specific tasks.
4. Train and Manage Change
- Train staff on platforms, faster and effectively using AI tools and capabilities.
- Engage stakeholders early and use structured change management strategies.
5. Monitor, Optimize, and Leverage Digital Twins
- Track KPIs like claims processing time and cost savings.
- Use process mining to analyze workflows and create a digital twin. Simulate and test process changes in the digital twin before implementation with full confidence.
- Continuously refine processes based on real and simulated insights.
- Expand BPaaS to telehealth, population health, and value-based care.
In a competitive landscape, GenAI super-powered BPaaS is not just a tool for survival but a strategy for thriving in the future of healthcare. By embracing advanced technologies and following a structured implementation roadmap, payers can now unlock unprecedented value.











