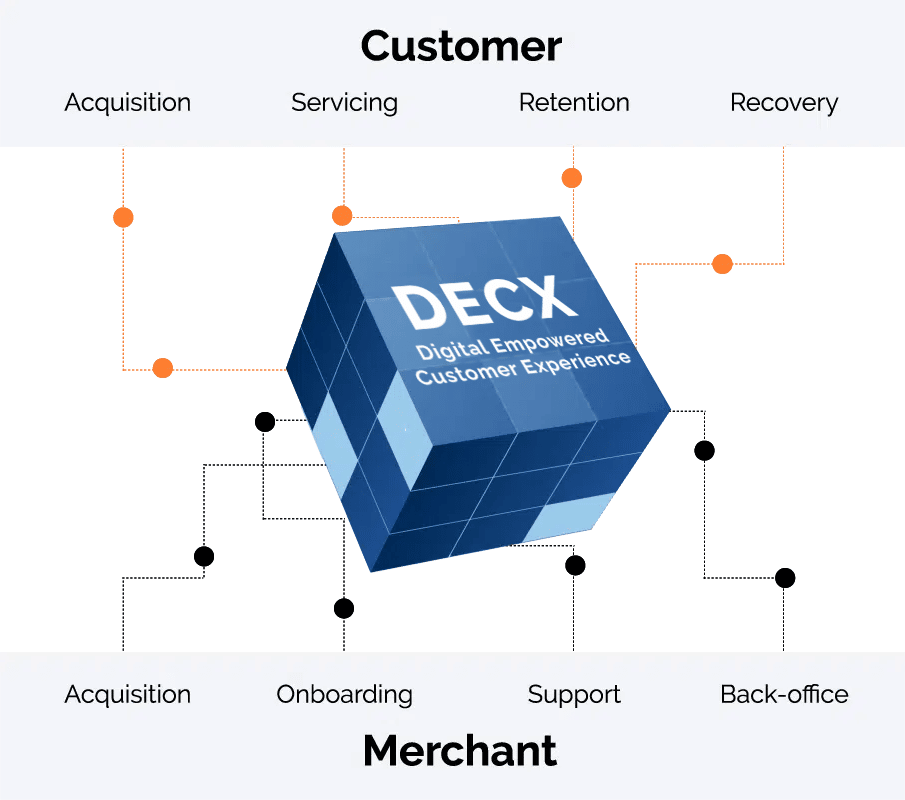
Digitally Empowered Customer Experience
Beyond the contact center: Design your customers’ experiences across the entire lifecycle
Customer relationships today are defined by a few fundamental truths:
- Customer experience (CX) has become a key differentiator. If you don’t get it right, another brand will.
- CX is the sum total of all the interactions that customers have with your brand. Only a small part of it happens in your contact center.
You won’t ever be in control of all the elements that make up CX. But: there are a bunch of new solutions out there to help you actively shape your customers’ experiences across many touchpoints today. That’s what DECX (digitally empowered customer experience) is all about.
Your customers are out there, everywhere. Where are you?
Customer relationships today are defined by a few fundamental truths:
- Customer experience (CX) has become a key differentiator. If you don’t get it right, another brand will.
- CX is the sum total of all the interactions that customers have with your brand. Only a small part of it happens in your contact center.
You won’t ever be in control of all the elements that make up CX. But: there is a bunch of new solutions out there to help you actively shape your customers’ experiences across many touchpoints today. That’s what DECX (digitally empowered customer experience) is all about.
We design experiences that work for your customers, your brand, and your business.
For Customer Services (CS) professionals this means a whole new set of KPIs to hit, in addition to the traditional ones: efficiency, FTR, and cost – meet perception, sentiment, renewal rates, and NPS. That’s a tall order. And it needs a customer experience (CX) strategy that’s a) operationally realistic, b) in line with your business goals, and c) supporting your Product, Sales and Marketing Departments’ efforts.
That’s what we help with.

How we do it
We use your real-life relationship data to fully understand your customer journeys from end-to-end.
Our Insights, Design Experience and Advisory practice applies human-centric design principles to genuinely put ourselves in your customers’ shoes.
We believe in the power of automation to deliver support quickly – and free agents to provide meaningful help in the moments that matter.
Learn more
Learn more
We believe in the power of automation to deliver support quickly – and free agents to provide meaningful help in the moments that matter.
We work with you to define what success will look like in your case. See how we are helping these brands actively shape their customer journeys…
customer experience
lift
efficiency
retention
experience
View Case Study
Achieved through faster transactions, and improved cross and upselling.
View Case Study
Automation and straight-through processing keep CX ops lean.
View Case Study
Higher NPS and customer-friendly processes have a positive impact on renewal rates.
View Case Study
Digitally empowered agents have the time and tools to solve real customer problems.
View Case Study
Digitally empowered agents have the time and tools to solve real customer problems.
Don’t just take our word for it. Take the analysts’, too
ISG, a leading advisory firm, have recently assessed the market for customer experience (CX) services and compared 28 providers. They named Firstsource a leader in Europe and the UK, across all four categories.
Dr. Kenn Walters,
Distinguished Lead Analyst, ISG
Firstsource has AI- and automation-driven platforms and solutions and significant domain expertise.
Enough with the visions. CX needs to work in the real world.
We’ve seen well-meaning customer experience (CX) strategies fail because they couldn’t translate their aspirational goals into operational reality. It’s time for CX realism – an approach that acknowledges that organizational change is hard – and addresses the obstacles real businesses face.
Digitally Empowered Customer Experience Solutions for Healthcare
Impress and delight your members with personalized and contextual services on a channel of their choice using digitally empowered customer experience (DECX) for Healthcare. It combines the best of what humans and technology have to offer to deliver the moments that matter across the member lifecycle – eligibility, onboarding, engagement and retention.
Explore CX insights:
Moments of delight:
How to translate operational excellence into powerful customer experiences
Talk to us
This form is for business inquiries. Click here for job applications and for employee reference checks.